The A to Z of Effective & Less Effective Immuno-Nutrients to Prevent and Combat Respiratory Tract & Other Infections
In their recent review in the Journal of the International Society of Sports Nutrition Vinicius Fernandes Cruzat, Maurício Krause and Philip Newsholme reviewed the extensive literature on nutritional supplements that act as immuno-nutrients, may to reduce immunosuppression and excessive inflammation in hard-training athletes and gymrats like yourself (or yourself in 2015 ;-)
Want to get stronger, bigger, faster and leaner, but not sick? Periodize appropriately!
"Although a balanced diet with high quality and sufficient quantity of nutrients is essential, there is growing evidence that some non-synthetic supplements can assist optimal nutrition. In fact, the use of nutritional supplements especially the provision of amino acids, has grown year-on-year. [...]As Cruzat et al. point out, the key targets for immunonutrition may include provision of key metabolites for immune cells per se. In other words: Immuno-nutrients feed the immune system and don't suppress but optimize the multi-layered immunte response consisting of
The use of proteins and amino acids for supplementation deserves special attention, since these molecules are critical for anti-oxidant and fuel provision, participating in the whole-body energy homeostasis, growth, development, recovery and immune responses.
- the inflammatory response and cytokine release,
- the production of chaperone proteins such as the heat shock proteins (HSPs),
- changes in the redox balance (including glutathione, GSH metabolism), and
- the protection of skeletal muscle mass (see Figure 1).
- Vitamin C: South African ultramarathon runners did demonstrate that vitamin C (but not E or beta-carotene)
supplementation (about 600 mg day7 1 for 3 weeks)
was related to fewer reports of upper respiratory tract infections (URTI) symptoms
(Peters 1983, 1990, 1993, 1996; Peters-Futre, 1997).
These beneficial effects have yet not been replicated by other research teams. Himmelstein, Robergs, Koehler, Lewis and Qualls (1998), for example, reported no alteration in URTI incidence among 44 marathon runners and 48 sedentary individuals randomly assigned to a 2 month regimen of 1000 mg /day of vitamin C or placebo. And in view of the fact that most randomized, placebo-controlled studies have been unable to demonstrate that vitamin C supplements modulate immune responses following heavy exertion (Nieman et al., 1997b, 2002b; Nieman, Peters, Henson, Nevines, & Thompson, 2000b), it should be clear that vitamin C must not be counted among the highly effective immune nutrients.
Classic ROS-scavengers like vitamin C are not just ineffective, when it comes to countering the increased susceptibility to infection they have also been shown to hamper the adaptational response to exercise | read more.
Zinc + C, not protetive, but effective? While the evidence supplementing with a combination of vitamin C and zinc would protect you from upper respiratory tract infections (URTIs) is scarce, there are studies like Maggini et al. (2012) which indicate that the provision of a
combination of 1000 mg vitamin C plus 10
mg zinc in patients with the common cold will lead to a nonsignificant reduction
of rhinorrhoea duration (range 9 – 27%)
was seen. Moreover, a pooled analyses of the two studies Maggini et al. conducted shows that "vitamin C plus zinc was
significantly more efficient than placebo at reducing rhinorrhoea over 5 days of treatment" (Maggini. 2012). Furthermore, symptom relief was quicker and the product was well
tolerated. Despite the fact that the subjects in these experiments were ordinary people, upping your zinc and vitamin C intake, when you've already caught a cold may help you to recover faster and thus get back to the grind earlier.
- Vitamin E: As Niemann et al. point out in their review of the efficacy of various immuno-nutrients, vitamin E functions primarily as a non-specific,
chain-breaking antioxidant that prevents the propagation of lipid peroxidation. The vitamin is a peroxyl
radical scavenger and protects polyunsaturated fatty
acids within membrane phospholipids and in plasma
lipoproteins.
The effect of vitamin E supplementation on the inflammatory and immune response to intensive and prolonged exercise is largely unstudied and equivocal. Cannon et al. (1991) found that vitamin E supplementation of 800 IU/day for 48 days attenuated endotoxin-induced IL-6 secretion from mononuclear cells for 12 days after running downhill on an inclined treadmill. Singh et al. (1999) showed no effect of vitamin E supplementation (4 days, 800 IU/day) on the increase in plasma IL-6 following a 98 min treadmill run at 65 – 70% V_ O2max to exhaustion. Petersen et al. (2002) reported no influence of vitamin E and C supplementation (500 mg and 400 mg, respectively, for 14 days before and 7 days after) on the plasma cytokine response to a 5% downhill 90 min treadmill run at 75% VO2max.
A 2004 study in the course of which triathletes competing in the Kona Triathlon World Championship race event received 800 IU/day of a-tocopherol for two months does even indicate that vitamin E can increase the degree of exercise induced lipid peroxidation and the amount of several cytokines in the blood following a triathlon.Against that background and in view of the previously cited ambiguous results, Niemann et al. (2006) rightly conclude that "vitamin E supplementation to counter immune suppression and oxidative stress in endurance athletes cannot be recommended" (Niemann. 2006).
Figure 2: Chronic supplementation with 800 IU of vitamin E (as alpha-tocopherol) has significant negative effects on markers of lipid oxidation and inflammation in triathletes (Nieman. 2004). - Vitamin D: For vitamin D a slightly different image emerges. It appears to be indisputable that athletes with low vitamin D levels are at higher risk of upper-respiratory tract infections - specifically during winter times (He. 2013).
The results of clinical trials investigating the benefits of vitamin D supplementation, however, are less unambiguous. In non-athletes, the monthly administration of 100 000 IU of vitamin D did not reduce the incidence or severity of URTIs; and that despite the fact that the supplement brought the 25OHD levels of the healthy subjects up, significantly (Murdoch. 2012). A meta analysis by Bergman et al. (2013), however indicates that "vitamin D has a protective effect against RTI, and dosing once-daily seems most effective".
Simply eating enough: It may sound funny, but in the end it's not surprising that a lack of readily usable energy makes you more susceptible to infections. Firstly, a general calorie restriction is often related to an insufficient intake of important micronutrients (Pendergast. 2002). And even if the intake of all micronutrients is adequate. Important immune factors such as glutamine are (ab-)used as a substrate to produce glucose in the liver and are thus no longer available to "feed" your immune cells. Accordingly it should not surprise you that Niemann and Bishop highlight in their review of "nutritional strategies to counter stress on the immune system in athletes" that the existing data indicates that "physiological
stress to some aspects of the immune system is
reduced when athletes use carbohydrate during
intense exertion lasting 90 min or more" and their own experiments suggest that this means "that athletes using carbohydrate beverages during competitive events will lower their risk of
sickness afterwards" (Nieman. 2006).
 |
| Figure 4: Mechanisms involving whey proteins as a source of different immunonutrients. (Cruzat. 2014). |
As you can see in Figure 4, Cruzat et al. put a particular emphasis on whey protein - for good reasons.
Firstly, whey contains all the "good" amino acids of which previous studies indicate that they may have direct beneficial effects on the immune system:
- Glutamine: As Cruzat et al. point out, "L-glutamine is probably the most widely recognized immuno-nutrient since it can be used as
an oxidizable fuel, a substrate for nucleotide synthesis, a modulator of intermediary
metabolism of amino acids, HSP expression and a component of GSH-mediated
antioxidant defense" (see Figure 5 | Cruzat. 2014).
Put simply glutamine is the food your immune cells thrive on. Accordingly scientists, athletes and coaches have speculated ever since the early 1990s that supplemental glutamine should be able to prevent the exercise induced immune impairments.
Why? Well, exercise depletes the amount of circulating glutamine and will thus "steal" the fodder your immune cells need to survive and function (Wernerman. 2008).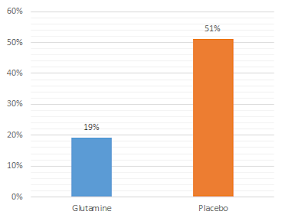
Figure 6: 5g of glutamine per day led to significant reductions in the occurrance of infections in marathon, ultra-marathon, mid distance runners and rowers (Castell. 1996a).
And in fact, there are studies that support the logical conclusion that the repletion of the glutamine that has been burned as alternative fuel during a workout with 0.1 g/kg body weight ameliorates the exercise induced reduction of lymphocytes, and could thus eventually reduce the risk of URTI’s (Castell. 1997).
In that, I deliberately used the conditional, because subsequent studies with fixed (20–30 g/day) or variable (0.3 - 0.5 g/kg body wt) doses of glutamine did not report similar outcomes (Castell. 1996b; Krzywkowski. 2001; Hiscock. 2002). Accordingly, Castell et al. write in their contribution to the BMJ A-Z Supplement review (ed. Newsholme. 2011):"Overall, there is no consensus or unifying concept to explain the efficacy of exogenous provision of glutamine alone on performance in athletes, although in combination with carbohydrate or other amino acids, significant improvements have been reported." (Newsholme. 2011)
In other words: Benefits can't be guaranteed, but specifically when glutamine is ingested in amounts of at least 20g/day in addition to carbohydrates and protein supplements it appears as if it could be a useful dietary supplement for hard-training athletes.
Where are all the other supplements gone? As I wrote in the introduction, this list is not supposed to be comprehensive. Furthermore, agents like quercetin, beta-glucan, curcumin or astragalus may be backed by animal studies, their efficacy in human beings does yet warrant further testing - specifically in athletes (Nieman. 2006). Other supplements such as the often-used herb Echinacea purpurea have been shown to fail to stimulate the nonspecific immune response and may be useful only when you are already sick or if the preperations are administered intravenously (Schwarz. 2002).
- Arginine: No, this is not a mistake. L-arginine is in fact the #2 on the list of supplemental immune modulators for hard-training athletes. Needless to say that it's not arginine itself, but rather Nitric Oxide (NO) which acts as a mediator of inflammation and immune system activation in the human body (Krause. 2011 & 2012).
As a SuppVersity reader, you know that arginine has little ergogenic effect. It has beneficial effects in diabetics and may offer benefits for people who want to control their blood pressure. As a immuno-modulator, however it is similarly ineffective as it is as an ergogenic. Benefits can only be expected if the blood levels of arginine are depleted and that is - even with heavy exercise - usually not the case.
- lactoferrin and lactoferricin, demonstrate direct anti-microbial activity and may thus protect you from infections,
- lysosome, lactoperoxidase and diverse globulins and peptides in whey provide a synergistic protective “cocktail” activity against viral and bacterial organisms (Ha. 2003), and
- sulphur-containing amino acids, such cysteine and taurine attenuate the reduction of intracellular GSH concentration induced by intensive exercise (Lands. 1999).
Bottom line: While there is good evidence for vitamin D supplementation (1,000-2,000IU/day in individuals with low levels and / or hard-working athletes during the winter months) and high doses of glutamine in hard working athletes. There is little doubt that the amino acid + protein + peptide coctail in whey proteins is the "goto supplement" you would choose if you wanted to use only one of the supplements discussed in this article.
In that, a reasonable dosage suggestion would be similar to that for maximal muscle hypetrophy and range from 20-60g per day - with the higher dosage being consumed in 2-3 servings evenly spread accross the day. Furthermore, studies like the one by Cury-Boaventura et al. (2008) indicate that, during periods of intense training, it may be useful to add glutamine. Either in large amounts of 10-20g per day (5-10g on top of each serving of whey) or, as it was the case in said study, as a dipeptide which has a higher chance of making it past the splachnic bed and not ending up as "fuel" for your organs and or glyconeogenic substrate in the liver.
And yes, if you've already caught a cold, 1 gram (in divided doses) of the the good old vitamin C (if you want to along with 5-15mg of zinc) is useful, as well - along with plenty of rest and sleep, of course ;-) Comment on Facebook!
References: |
| Whey Beyond Brawn: 10+ Things You Probably Didn't Know Whey & Peptides That Form During its Digestion Can Do | learn more. |
And yes, if you've already caught a cold, 1 gram (in divided doses) of the the good old vitamin C (if you want to along with 5-15mg of zinc) is useful, as well - along with plenty of rest and sleep, of course ;-) Comment on Facebook!
- Cury-Boaventura, Maria Fernanda, et al. "Effects of exercise on leukocyte death: prevention by hydrolyzed whey protein enriched with glutamine dipeptide." European journal of applied physiology 103.3 (2008): 289-294.
- Bergman, Peter, et al. "Vitamin D and respiratory tract infections: a systematic review and meta-analysis of randomized controlled trials." PloS one 8.6 (2013): e65835.
- Castell, L. M., E. A. Newsholme, and J. R. Poortmans. "Does glutamine have a role in reducing infections in athletes?." European journal of applied physiology and occupational physiology 73.5 (1996a): 488-490.
- Castell, L. M., et al. "Some aspects of the acute phase response after a marathon race, and the effects of glutamine supplementation." European journal of applied physiology and occupational physiology 75.1 (1996b): 47-53.
- Castell, Linda M., and Eric A. Newsholme. "The effects of oral glutamine supplementation on athletes after prolonged, exhaustive exercise." Nutrition 13.7 (1997): 738-742.
- Cruzat, Vinicius F., et al. "Amino acid supplementation and impact on immune function in the context of exercise." Journal of the International Society of Sports Nutrition 201.4 (2014): 11:61.
- Cury-Boaventura, Maria Fernanda, et al. "Effects of exercise on leukocyte death: prevention by hydrolyzed whey protein enriched with glutamine dipeptide." European journal of applied physiology 103.3 (2008): 289-294.
- Ha, Ewan, and Michael B. Zemel. "Functional properties of whey, whey components, and essential amino acids: mechanisms underlying health benefits for active people (review)." The Journal of nutritional biochemistry 14.5 (2003): 251-258.
- He, Cheng-Shiun, et al. "Influence of vitamin D status on respiratory infection incidence and immune function during 4 months of winter training in endurance sport athletes." Exerc Immunol Rev 19 (2013): 86-101.
- Hiscock, Natalie, and Bente Klarlund Pedersen. "Exercise-induced immunodepression–plasma glutamine is not the link." Journal of Applied Physiology 93.3 (2002): 813-822.
- Lands, L. C., V. L. Grey, and A. A. Smountas. "Effect of supplementation with a cysteine donor on muscular performance." Journal of Applied Physiology 87.4 (1999): 1381-1385.
- Krause, Mauricio S., et al. "L-arginine is essential for pancreatic β-cell functional integrity, metabolism and defense from inflammatory challenge." Journal of endocrinology 211.1 (2011): 87-97.
- Krause, Mauricio, et al. "Differential nitric oxide levels in the blood and skeletal muscle of type 2 diabetic subjects may be consequence of adiposity: a preliminary study." Metabolism 61.11 (2012): 1528-1537.
- Kreider, Richard B., et al. "Effects of ingesting protein with various forms of carbohydrate following resistance-exercise on substrate availability and markers of anabolism, catabolism, and immunity." Journal of the International Society of Sports Nutrition 4.1 (2007): 1-11.
- Maggini, S., S. Beveridge, and M. Suter. "A combination of high-dose vitamin C plus zinc for the common cold." Journal of International Medical Research 40.1 (2012): 28-42.
- Murdoch, David R., et al. "Effect of Vitamin D3 Supplementation on Upper Respiratory Tract Infections in Healthy AdultsThe VIDARIS Randomized Controlled TrialVitamin D3 and Upper Respiratory Tract Infections." Jama 308.13 (2012): 1333-1339.
- Newsholme, Philip, et al. "BJSM reviews: A to Z of nutritional supplements: dietary supplements, sports nutrition foods and ergogenic aids for health and performance—Part 18." British journal of sports medicine 45.3 (2011): 230-232.
- Nieman, David C., et al. "Vitamin E and immunity after the Kona triathlon world championship." Medicine and science in sports and exercise 36 (2004): 1328-1335.
- Nieman, David C., and Nicolette C. Bishop. "Nutritional strategies to counter stress to the immune system in athletes, with special reference to football." Journal of sports sciences 24.07 (2006): 763-772.
- Nieper, A. "Nutritional supplement practices in UK junior national track and field athletes." British journal of sports medicine 39.9 (2005): 645-649.
- Pendergast, David R. "Effect of dietary intake on immune function in athletes." Sports medicine 32.5 (2002): 323-337.
- Schwarz, Eveline, et al. "Oral administration of freshly expressed juice of Echinacea purpurea herbs fail to stimulate the nonspecific immune response in healthy young men: results of a double-blind, placebo-controlled crossover study." Journal of Immunotherapy 25.5 (2002): 413-420.
- Waldron, Jenna Louise, et al. "Vitamin D: a negative acute phase reactant." Journal of clinical pathology (2013): jclinpath-2012.
- Wernerman, Jan. "Clinical use of glutamine supplementation." The Journal of nutrition 138.10 (2008): 2040S-2044S.












